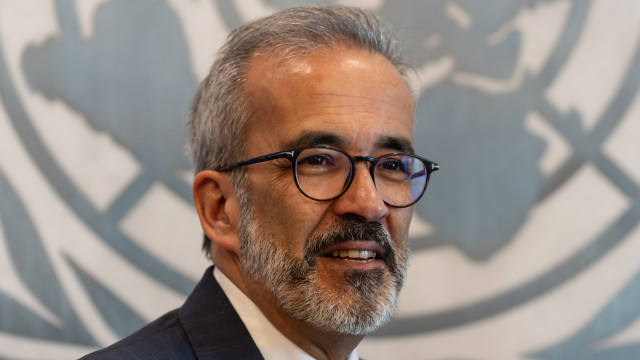
“Unlike any other specialty – and I have serious doubts about its legality – occupational medicine is the only one that has a weekly working hours limit. By law, an occupational physician can work only 37.5 hours a week,” stated the president of the Occupational Medicine College of the Order of Physicians to Lusa agency.
The issue revolves around the Legal Framework for the Promotion of Safety and Health at Work, a 2009 law stipulating that occupational doctors “are prohibited from ensuring the health surveillance of a number of workers corresponding to more than 150 hours of activity per month,” with any breach of this limit subject to severe penalties.
If there were no legal limit of 37.5 working hours a week, the current shortage of occupational medicine specialists would no longer exist in the country, highlighted Maria José Almeida.
“If an occupational doctor could work the same hours as any other medical specialty, there would no longer be this limitation,” said the president of the college, noting that the specialty also faces an older average age of practitioners, predominantly concentrated in urban centers and coastal areas.
According to the Green Book of the Future of Safety and Health at Work, the specialty is among the most aged, with a significant proportion of doctors aged 60 or above, and struggles with a limited number of annual places for medical internship.
“Every year the available places are increasing, but we are trying, internally and with the Central Administration of the Health System (ACSS), to review our training plan to allow a substantial increase in numbers over the coming years to help bring more doctors into the market,” stated the specialty college president.
Maria José Almeida stated that a study by the Order of Physicians indicates around 50 doctors should enter specialized training annually, whereas in practice it’s about 30.
The specialist acknowledged that this is not the ideal number but emphasized the need to ensure “that training eligibility services genuinely have the conditions to receive and train internal doctors over four years with quality.”
“Currently, all possible sites to host internal doctors already have the eligibility and are almost operating at their full capacity. Therefore, we need Local Health Units to open internal services so that we can train more doctors nationwide,” she said.
Highlighting it as a “passionate specialty” practiced about 90% in companies, Maria José Almeida argued that occupational medicine has the pull to attract new doctors as it offers “broad training and the possibility to work in diverse locations.”
“An occupational doctor can simultaneously work in a tuna factory, a shoe factory, a shipyard, and a hospital and deal with diverse pathologies, as our focus is not a patient but a worker,” explained the specialist.
The president of the occupational medicine college recognized that most companies still view occupational medicine as a legal obligation, but expressed belief that, in the near future, awareness will increase regarding the benefits of disease prevention, accident prevention, and productivity gains.
Concerning occupational diseases, Maria José Almeida noted that musculoskeletal disorders are the most diagnosed, yet since the COVID-19 pandemic, there has been increased attention from occupational doctors toward psychosocial pathologies.
“There is an increase in these diagnoses, which does not mean that people are now more mentally ill than years ago, but that there is a different awareness,” she stated.
From the workers’ perspective, Maria José Almeida warned that considering the high number of people without a family doctor in certain regions, the “occupational doctor is, in many circumstances, the only one with whom they have contact.”
“The feeling I have – working in a Local Health Unit and at a corporate level – is that people see many benefits because they feel heard and understood from the company’s perspective,” the doctor emphasized.