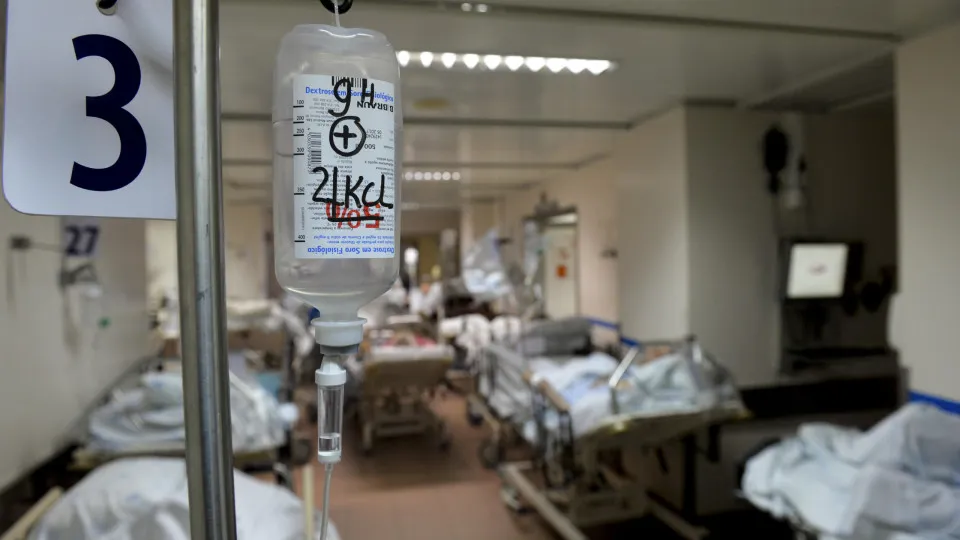
A recent index reveals that all 31 hospitals in the National Health Service (NHS) that responded (out of a total of 43) are experiencing medication shortages, with more than half facing these issues daily or weekly.
In 61% of reported cases, the shortage’s impact was severe, 18.5% involved all types of medications, and 13.42% primarily affected generics or biosimilars. In 23% of instances, there was a need to alter patient treatment due to the lack of certain drugs.
“The problem has been escalating,” stated Xavier Barreto, president of the Portuguese Association of Hospital Administrators (APAH), acknowledging the disturbances already affecting patients.
Barreto stressed that this situation should serve as “a warning to the Government,” adding, “In the future, we must scrutinize this matter further to understand which specific medications are missing and why.”
“We will need to analyze in greater detail to determine what specific actions can be taken,” he added.
The impacts of these shortages as cited by hospitals include treatment delays (17%), therapeutic changes (67%), and either treatment delays/suspensions or therapeutic changes (17%).
On a scale from 0 to 100, over 80% of hospitals rated access to innovative drugs at 75 points. However, the index for innovation access has been declining since 2018 (77%), reaching 54% last year.
Regarding barriers to medication access, about one-third of units feel the procurement process is never initiated promptly, although only 19% reported that pricing or financing model was a barrier to accessing any medication.
Most institutions (90%) have cost-control strategies for medications, such as specific policies for biosimilar management, automatic substitution by International Nonproprietary Name (INN) in the pharmacy, price negotiations with the industry, or issuing prescription guidelines.
Administrative burden (42%), inefficiency in the Ministry of Health’s Shared Services (25%), and lack of financial authorizations (14%) were identified as the most relevant barriers. There was no mention of an absence of authorization from the Administrative Board.
The majority of hospitals utilize medications before the funding decision, ensuring overarching access to therapeutic innovation.
Once the funding decision is made, in most institutions (80%), access to medication occurs only after it is included in the National Drug Formulary (FNM).
For medications where financing is based on risk-sharing mechanisms and result monitoring related to that sharing, 84% of institutions already monitor these outcomes.