Identified for the first time in Brisbane in 1994, the Hendra virus infects people in Australia through horses and a species of bat in eastern Australia known as the “flying fox,” while outbreaks of the Nipah virus occur almost annually in Bangladesh and occasionally in other Asian countries where it is transmitted by bats.
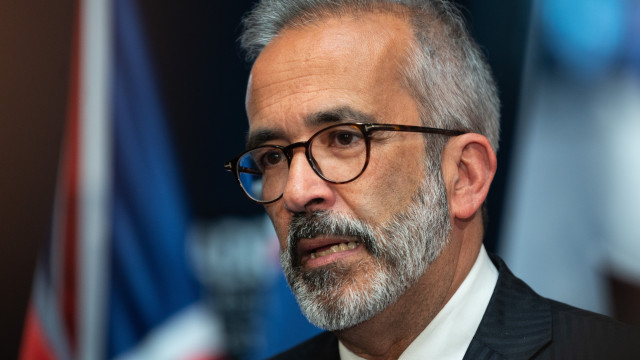
A team of scientists from Chile, Australia, and China has discovered a nanobody capable of combating these henipaviruses.
The details of the discovery were published on Tuesday in the journal Nature Structural & Molecular Biology.
“A nanobody is one-tenth the size of an antibody, and because it is so small, it can access hard-to-reach areas of the virus to block infection,” explained the study coordinator, Ariel Isaacs, from the University of Queensland (UQ, Australia).
Furthermore, “nanobodies are also easier to produce and more stable at higher temperatures than traditional antibodies, so we are very excited about the potential of our discovery to lead to new treatments,” emphasized the scientist.
The nanobody, named DS90, was part of a series isolated by a team of scientists from the Austral University in Chile from the immune cells of an alpaca named Pedro.
Camelids, including alpacas, are the only terrestrial animals that produce nanobodies.
DS90 was identified through a platform developed by Professor Alejandro Rojas-Fernández, which allows the isolation of nanobodies against concerning viruses.
“Together with UQ, our goal was to build a broad barrier against future pandemic viruses based on scalable antiviral nanobodies. This fantastic work is just the beginning,” assured Rojas-Fernández.
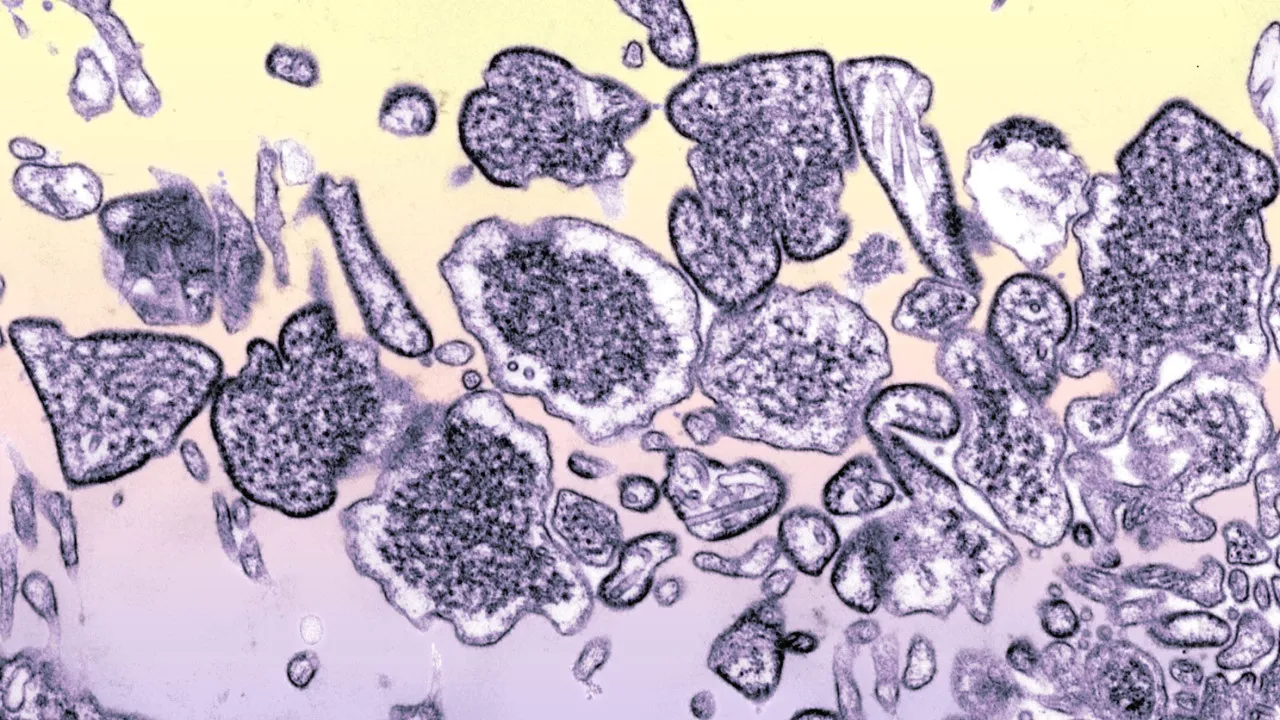
Tests conducted in the laboratory of Daniel Watterson at the School of Chemistry and Molecular Biosciences at the University of Queensland confirmed that DS90 successfully bound to the proteins of the Nipah and Hendra viruses, blocking their ability to enter cells.
Using cryogenic electron microscopy, the team managed to examine the process and see “exactly how the nanobody binds to the virus, reaching deep within, while antibodies normally only bind to the exposed surfaces of viruses,” explained Watterson.
“This new information is a crucial step towards using a nanobody to combat the Hendra and Nipah viruses, which cause outbreaks in humans and can often lead to fatal respiratory and neurological diseases,” noted the researcher.
In addition, the team combined the DS90 nanobody with a developing antibody therapy, used as a last resort treatment for people infected with Hendra and Nipah.
The team demonstrated that the combination of DS90 with the m102.4 antibody, manufactured at UQ, prevents the mutation and evolution of the Nipah virus.
Some nanobodies have been approved for use in cancer treatments, and now “it is exciting to see that nanobodies can also be used to neutralize viruses,” added the scientist.
The next step will be to translate the findings into a treatment ready for clinical use in the event of a Hendra outbreak in Australia or Nipah in Asia.